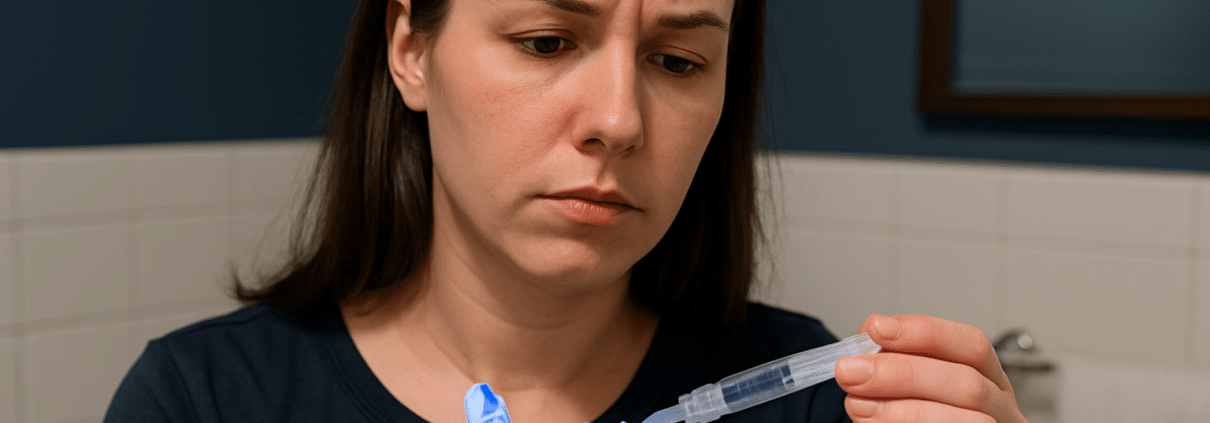
The promise is seductive: Whiten your teeth in days for less than dinner in LA. No dentist, no downtime, just whiter teeth in your bathroom mirror. But before you click add to cart on those OTC whitening kits, it’s worth pausing to ask: are they actually safe? Do they work—or just wear down your enamel while you wait for results?
The booming market of over-the-counter teeth whitening is flooded with LED kits, strips, pens, and pastes. Some are effective. Some are useless. And some can leave your teeth worse off than when you started. Here’s what you need to know before you DIY your smile.
TLDR – Quick Guide
- OTC whitening kits can offer mild to moderate whitening results—but not all are created equal.
- Ingredients and concentrations matter. Many kits are weaker than professional options.
- Misuse can lead to tooth sensitivity, enamel damage, or gum irritation.
- Consult a dentist before starting if you have crowns, fillings, or gum issues.
- For real results and less risk, supervised whitening (even take-home trays) is often the smarter move.
Detailed Breakdown: Are OTC Whitening Kits Safe?
1. What Are OTC Whitening Kits Made Of?
Most OTC whitening kits use either hydrogen peroxide or carbamide peroxide as their active ingredients. These bleaching agents work by breaking down stains into smaller, less visible particles.
The difference? Hydrogen peroxide acts faster but fades quicker. Carbamide peroxide works slower but is gentler.
Some trendy kits also include baking soda, LED lights, or even charcoal—not all of which are backed by science.
2. Are They FDA-Approved or Dentist-Recommended?
Here’s the thing: the FDA does not regulate whitening kits as medical devices, so quality control is hit or miss. Some OTC kits from reputable brands (like Crest Whitestrips) have solid clinical backing. Others, especially knockoffs sold through social media, are less transparent—and riskier.
A 2021 study in the Journal of Esthetic and Restorative Dentistry found that improper OTC kit use could lead to enamel surface roughness and mineral loss.
3. Common Side Effects to Watch For
- Tooth Sensitivity: Especially in kits with high peroxide levels or prolonged use
- Gum Irritation: If the gel contacts soft tissue
- Uneven Whitening: Most OTC kits are one-size-fits-all, which can cause patchy results
- Enamel Erosion: With overuse or improper application
4. When to Avoid OTC Whitening Kits
Skip the kits—or at least consult your dentist first—if you have:
- Crowns, veneers, or fillings (they won’t whiten)
- Gum disease or exposed roots
- Tooth sensitivity
- Pregnant or nursing (better safe than sorry)
Instead, consider custom take-home trays or in-office options, which are safer and more controlled.
5. What Actually Works?
If you’re set on going the OTC route, look for:
- ADA Seal of Acceptance
- Clear peroxide percentage (5–10% is typical for OTC, 15–40% for pro use)
- Gum protection like custom-fit trays or desensitizing agents
For better results, dentists like Valery Sweeny, DDS offer both in-office whitening and custom trays with professional-grade gel—without the risks of a misfire.
Key Takeaways
- OTC whitening kits can be effective—but only when used correctly and cautiously.
- The strength and delivery method matter more than flashy branding.
- If you have dental work or underlying issues, OTC whitening can backfire.
- To minimize risks, consult your dentist or consider professional-grade take-home options.
- Your smile deserves more than a roll of the dice from a TikTok ad.
FAQs
Are OTC whitening kits bad for your enamel?
They can be if misused or overused. Always follow instructions and avoid daily use unless directed by a dentist.
How long do results from OTC kits last?
Usually a few months, depending on your diet and habits. Smoking, coffee, and red wine will shorten results.
Can I use an OTC kit if I have sensitive teeth?
Proceed with caution. Choose low-peroxide products and stop use if pain occurs.
Do LED lights in whitening kits actually help?
Not significantly, according to most dental research. The peroxide does the heavy lifting, not the light.
Can I combine OTC kits with professional whitening?
You shouldn’t. Doubling up can lead to over-bleaching and sensitivity. Stick to one method at a time.
Let’s be honest—life happens. Between work, kids, anxiety, or just not knowing where to start, dental care sometimes falls to the bottom of the list. If you’ve neglected your teeth for years, you might be dealing with shame, pain, or fear of judgment. But here’s the truth: you’re not the only one. And more importantly—you’re not beyond help.
Modern dentistry is built for comebacks, not criticism. Whether it’s been 3 years or 30, there’s a path back to health, function, and confidence. And it’s easier (and less scary) than you think.
TLDR – Quick Guide
- Neglecting dental care can lead to decay, gum disease, tooth loss, and systemic health issues.
- Many people delay visits due to fear, cost, or embarrassment.
- Today’s dental practices prioritize comfort, privacy, and nonjudgmental care.
- Treatments like deep cleaning, crowns, implants, and full-mouth restorations can rebuild your smile.
- Practices like Valery Sweeny, DDS in Los Angeles specialize in compassionate, results-driven smile makeovers.
Implementation Tactics: What to Expect If You’ve Neglected Teeth for Years
1. Start with a Judgment-Free Dental Exam
The first step is a comprehensive exam. You’ll get digital x-rays, a gum health check, and a one-on-one conversation with your dentist—without shame or lectures. This is about figuring out where you are and where you want to go.
At Valery Sweeny, DDS, patients are treated like partners—not problems.
2. Deep Cleaning (Scaling and Root Planing)
If your gums bleed or feel sore, you may have gingivitis or periodontitis. Deep cleanings remove years of tartar and bacteria buildup, allowing gums to heal and inflammation to subside.
- Why it matters: Gum disease is the #1 cause of tooth loss in adults.
- What it feels like: Mild discomfort, but you’ll feel so much better after.
3. Restorative Work: Fillings, Crowns, and Root Canals
Once decay is under control, it’s time to save or rebuild what’s left. Cavities are filled, broken teeth are crowned, and infected roots are treated.
- Pro tip: With numbing and sedation options, procedures are now virtually pain-free.
4. Tooth Replacement: Implants, Bridges, or Dentures
Missing teeth? No problem. Options range from individual implants to implant-supported dentures or bridges that feel natural and look amazing.
- Don’t worry: You won’t walk out toothless. Temporary solutions are always available during the transition.
5. Cosmetic Upgrades
Once your mouth is healthy, you can level up with whitening, veneers, or Invisalign. But those come after function and health are restored—not before.
Common Reasons People Avoid the Dentist
Understanding the why behind dental neglect helps eliminate shame:
- Dental Anxiety: Past trauma or fear of pain
- Financial Constraints: No insurance or fear of high costs
- Embarrassment: Fear of being judged for the condition of your mouth
- Busy Lives: Life, work, and caretaking responsibilities
Today’s dental offices get it. Providers like Valery Sweeny, DDS offer flexible payment plans, sedation options, and compassionate staff to help you feel safe.
What Recovery Looks Like
- Visit #1: Comprehensive exam and x-rays
- Visit #2: Deep cleaning or urgent repairs
- Phase 1: Restore function—treat decay, infection, missing teeth
- Phase 2: Improve aesthetics—whitening, alignment, veneers if desired
- Ongoing: Preventive care every 6 months
You don’t have to fix everything at once. Treatment is paced to fit your comfort level, budget, and lifestyle.
Key Takeaways
- Neglecting your teeth for years is more common than you think—and always reversible.
- Your first visit is about understanding your needs, not judging your past.
- Step-by-step care can restore your health, appearance, and confidence.
- Treatments are more comfortable, modern, and accessible than ever.
- Practices like Valery Sweeny, DDS in LA specialize in smile makeovers for patients who’ve been out of the dental chair for a while.
FAQs
Will my dentist judge me if I haven’t been in years?
A good dentist won’t. Offices like Valery Sweeny, DDS focus on progress, not the past.
How many visits will it take to fix my teeth?
It depends on your condition, but most patients see improvements within a few appointments. Major restorations may take a few months.
Can I get sedation if I’m nervous?
Absolutely. Many practices offer laughing gas, oral sedation, or even IV options.
Is this going to cost a fortune?
Not necessarily. Payment plans and phased treatments can help spread out costs. Always ask for a written treatment plan.
Is it too late to save my teeth?
Rarely. Even severely damaged mouths can be restored with the right treatment plan.
You’re doing the “right” thing—flossing daily like your dentist says—and suddenly, there’s blood. Cue panic. Should you stop? Push through? Call 911? Not quite.
While bleeding gums might seem like a red flag (literally), they’re not uncommon. But that doesn’t mean they should be ignored. If your gums bleed when flossing, your body’s trying to tell you something—and this blog is your cheat sheet to decoding that message.
TLDR – Quick Guide
- Bleeding gums when flossing is often due to inflammation from plaque buildup or improper technique.
- It can also be a sign of gum disease, vitamin deficiency, or even hormonal shifts.
- Mild bleeding that resolves with better hygiene is normal. Ongoing or painful bleeding isn’t.
- Professional cleanings and exams can catch and treat underlying issues early.
Detailed Breakdown: Why Your Gums Might Bleed When Flossing
1. Gingivitis: The #1 Culprit
When plaque sits along the gumline, your body reacts with inflammation. This is gingivitis, and bleeding is often its first symptom. It’s reversible, but if ignored, it can evolve into full-blown gum disease.
According to the CDC, nearly 50% of adults over 30 have some form of periodontal disease.
2. You Just Started Flossing Again
If flossing isn’t your daily habit, starting up again can irritate gums and cause minor bleeding. Think of it like sore muscles after a workout. Keep going—gently—and it should stop within a week.
3. Poor Flossing Technique
Aggressive flossing or snapping the string into your gums does more harm than good. Proper flossing involves gliding the floss gently between teeth and hugging each side.
4. Vitamin Deficiencies (Especially Vitamin C and K)
Your gums need nutrients, too. A lack of vitamin C can lead to inflamed, bleeding gums, while vitamin K is crucial for blood clotting. Diets low in fresh produce or those with absorption issues may be at risk.
5. Hormonal Changes
Pregnancy, menstruation, and menopause can all increase gum sensitivity due to hormonal fluctuations. “Pregnancy gingivitis” is real and affects many women.
6. Gum Disease (Periodontitis)
If the bleeding is accompanied by gum recession, persistent bad breath, or loose teeth, it may be periodontitis—a serious gum infection that requires professional treatment.
7. Medications
Blood thinners, anti-inflammatories, and certain anti-seizure medications can make gums more prone to bleeding. Always tell your dentist about any prescriptions you’re taking.
When to See a Dentist
If your gums bleed when flossing for more than a week—even with perfect technique—it’s time to get evaluated. Red flags include:
- Swelling or pain
- Bleeding while brushing
- Receding gums
- Persistent bad breath
- Loose teeth
Clinics like Valery Sweeny, DDS in Los Angeles specialize in identifying early gum issues and providing personalized care before it escalates into something worse.
How to Fix It: Smart Steps to Stop the Bleeding
- Improve Technique: Use a gentle, C-shaped motion when flossing.
- Stay Consistent: Floss daily, even if you’re bleeding—it should improve over time.
- Upgrade Your Tools: Soft-bristled toothbrushes and waxed floss can reduce irritation.
- Clean Professionally: Schedule a dental cleaning to remove tartar and plaque.
- Check Your Diet: Add more leafy greens, citrus fruits, and vitamin-rich foods.
- Talk to Your Dentist: Especially if you’re on medications or have chronic symptoms.
Key Takeaways
- Bleeding gums during flossing are usually caused by inflammation or poor technique.
- It’s often the first sign of gingivitis—and a warning to step up your oral care.
- Hormonal changes, diet, and medications can also play a role.
- If bleeding lasts more than a week, get it checked—especially if there are other symptoms.
- Dental offices like Valery Sweeny, DDS in LA offer preventative and periodontal care to keep gums healthy long-term.
FAQs
Should I stop flossing if my gums bleed?
No. Keep flossing gently. The bleeding often subsides after a few days of consistent care.
How long should I give it before seeing a dentist?
If bleeding persists for more than 7–10 days, book a dental exam.
Is bleeding always a sign of gum disease?
Not always. It can be from flossing too aggressively or hormonal changes—but it should still be evaluated if it continues.
Can I use a water flosser instead?
Yes. Water flossers are gentle on the gums and can be a great alternative, especially for sensitive mouths.
What if only one area bleeds when I floss?
That could signal localized irritation or an issue like a cavity or tartar buildup. Get it checked out.